Research
The breakthroughs in vision research and treatment we are helping to pioneer are substantial. Several procedures have been developed that have resulted in restoring eyesight to some individuals who had lost it through disease or trauma. In addition, we are exploring new ways to bring rehabilitation services to millions of people who are affected by low vision.
From researching diseases such as glaucoma and cataracts, to studying how scar tissue forms in the eye, we are discovering new treatments through partnerships with researchers worldwide.
And as the Foundation continues to grow, programs designed to foster similar hearing loss treatments will be developed. Every day brings new advances, and every breakthrough brings new hope.
Read about our Medical Breakthroughs
Read about our Research Projects
Research Discoveries
When these research breakthroughs are fully implemented into patient care, the Foundation is confident that millions of years of lost eyesight will be saved, and that cost savings to public health and productivity will have been made for pennies on the dollar. That is the power of the modern biomedical research era that began in the 1960’s, toward the end of Helen Keller’s life.
PEELING THE MACULA
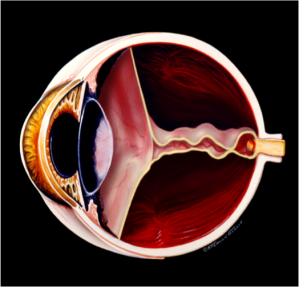
As the twentieth century concluded, with Time magazine naming Helen Keller as one of the century’s 100 most important figures, the Helen Keller Foundation completed its first decade of work in her name. Foundation researchers first reported a revolutionary surgery to repair the diseased macula, the human center of vision (Figure 1). Click For References
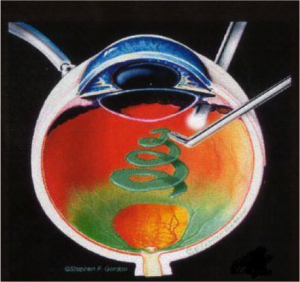
Figure 1. Peeling the Internal Limiting Membrane (ILM) of the Macula (the human center of vision). ©Stephen F. Gordon.
TEMPORARY KERATOPROSTHESIS (TKP) VITRECTOMY FOR THE INJURED EYE
The Foundation proved that recently injured eyes with no remaining light perception (NLP) could often be surgically restored to useful vision (Figure 2), saving many eyes from being removed without benefit of exploration and attempted reconstruction. Click For References
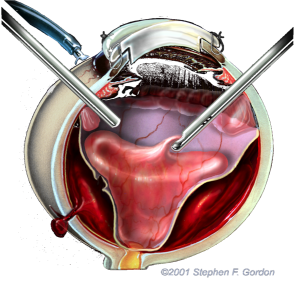
Figure 2. Temporary Keratoprosthesis (TKP) Vitrectomy – An optical device inserted in place of an injured cornea provides temporary surgical visualization of the posterior eye for vitrectomy reconstruction. ©Stephen F. Gordon
LASER CERCLAGE FOR THE PREVENTION OF RETINAL DETACHMENT
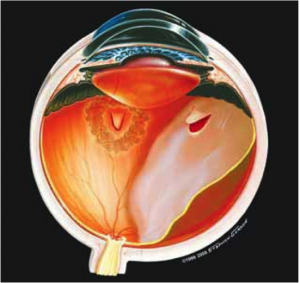
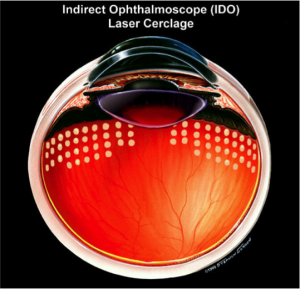
Spontaneous retinal detachment in the aging eye has plagued mankind since ancient times, producing blindness that became partially treatable only in modern times (Figure 3a). In 2002, Foundation researchers announced a laser treatment that prevented retinal detachment in high risk eyes with 98% certainty (Figure 3b).Click For References
Figure 3a. Spontaneous retinal detachment in the aging eye. @1999 Stephen F. Gordon
Figure 3b. Ora Secunda Cerclage (OSC) – non invasive laserspots prevent retinal detachment in high risk eyes. ©1999 Stephen F. Gordon.
RETINAL DETACHMENT PROPHYLAXIS IN EYES UNDERGOING PERMANENT KERATOPROSTHESIS (KPRO)
SILICONE OIL PREVENTION OF PROLIFERATIVE VITREORETINOPATHY (PVR)
For those who have already suffered retinal detachment, the Foundation has also developed a surgical treatment that dramatically reduces scar tissue complications (PVR) in retinal detachment repair (Figure 4a and 4b). Click For References
Figure 4a. Scar tissue detaches the retina, pulling it to the center of the eye.©Stephen F. Gordon.
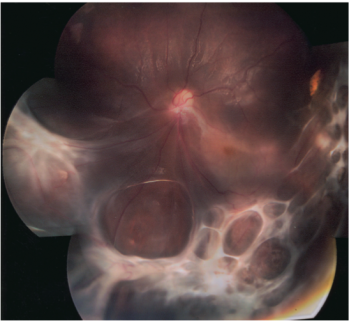
Figure 4b. Actual photograph of PVR scar tissue injuring the retina.
MACULOPEXY© FOR DIFFUSE DIABETIC MACULAR EDEMA
The new maculopexy procedure permanently increases tissue resistance to swelling, as an alternative to long-term drug injection therapy. Click For References
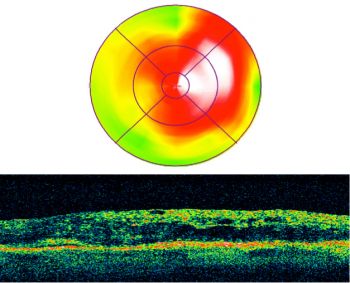
Figure 5a. Preoperative image of a swollen center of vision (macula), visual acuity 20/60.
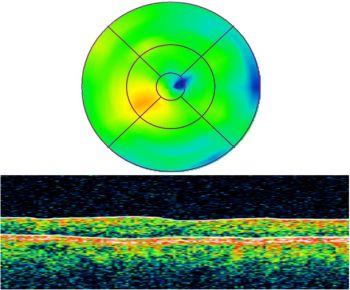
Figure 5b. Four years postoperatively, the macula is still dry and reading vision is restored to 20/20.
VITREOUS OPACITY VITRECTOMY
In 2007, the Foundation introduced the first safe and effective treatment for severe vitreous floaters to be honored by a major eye surgery society, the American Society of Retina Specialists. We named this Degenerative Vitreous Syndrome, or Vitreous Opacity Syndrome (VOS). Vitreous Opacity Vitrectomy is now finally bringing hope to “floater” sufferers who have substantial interference with activities of daily living (Figure 6). Click For References
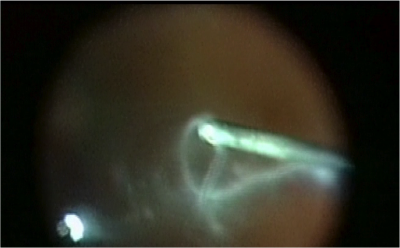
Figure 6. A photo captures cloudy vitreous “floaters” being removed by vitrectomy.
MACULOPEXY FOR THE TREATMENT OF BRANCH RETINAL VEIN OCCLUSION (BRVO)
Second only to diabetic retinopathy, Branch Retinal Vein Occlusion (BRVO), or a stroke of the retina, is the most common form of blood vessel problems affecting the eye and causing vision loss.7 The macula, the human center of vision, is severely injured in most cases of BRVO (Figure 7a). Helen Keller Foundation researchers have developed a laser-based surgical technique that permanently cures severe macular swelling (edema) after BRVO, usually returning macular vision to near normal (Figures 7b and 7c).
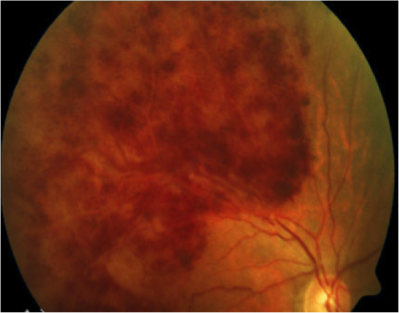
Figure 7a. Fundus image of affected retina in BRVO.
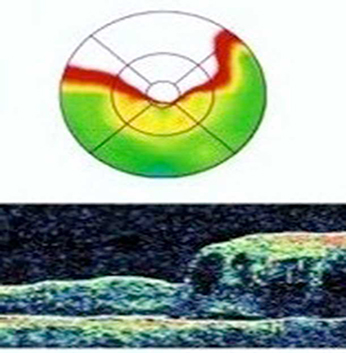
Figure 7b. Preoperative OCT of BRVO. Visual acuity 20/80
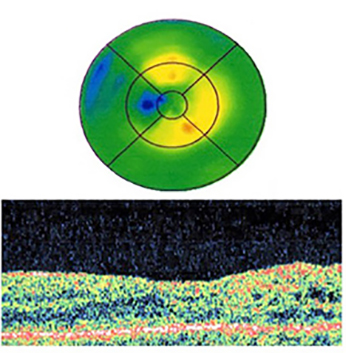
Figure 7c. 8-months postoperative. Visual acuity 20/40
MOBILIZE AND MOVE (M&M) VITRECTOMY© FOR SUBMACULAR HEMORRHAGE
Sudden and severe hemorrhage in a patient with macular degeneration. The Foundation’s M&M Vitrectomy quickly moves the clot out of the macula, usually restoring reading visual acuity. Click For References
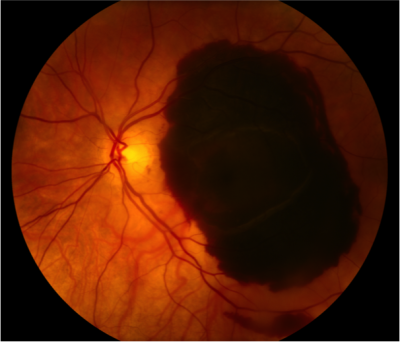
Preoperative Visual Acuity, Count Fingers
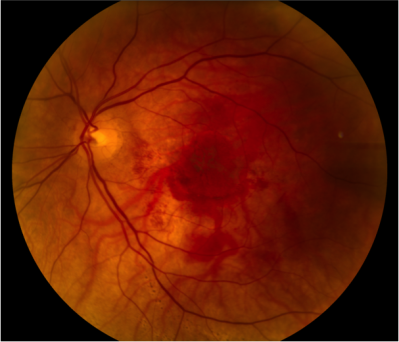
Postoperative 3 months, Visual Acuity 20/20
COMPLETE AND EARLY VITRECTOMY FOR ENDOPHTHALMITIS (CEVE) FOR THE TREATMENT OF POSTOPERATIVE ENDOPHTHALMITIS (POE)
Cataract extraction is perhaps the most successful operation of all time in restoring quality of life to those affected. But infection (endophthalmitis) can occasionally appear inside the eye after surgery, usually destroying vision within a few days if not successfully treated (Figure 9a). Helen Keller Foundation researchers have developed a new surgical debridement technique and an associated treatment paradigm that quickly restores a clear, non-toxic environment inside the infected eye (Figure 9b). This leads to rapid and maximal vision recovery. Click For References
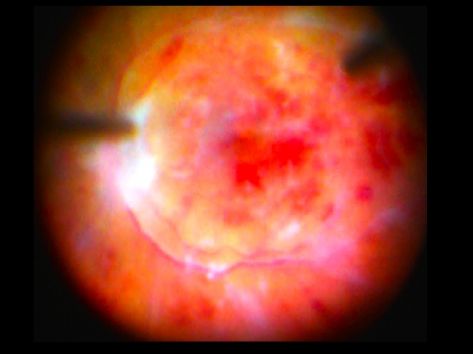
Figure 9a. Intraoperative image of Advanced Endopthalmitis Retinopathy
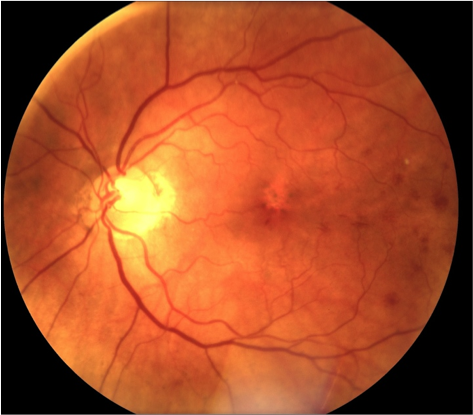
Figure 9b. Image of clear fundus 3-weeks postoperative.